Dear Dr. Sanjay Gupta,
I take great exception to your recent Twitter tweet.
"this is a meningioma, a benign brain tumor. once removed, patient is cured."
Who knew it was that simple?
I've responded to your blog, but my letter must still be under moderator consideration as it has yet to post. Allow me to share with you now.
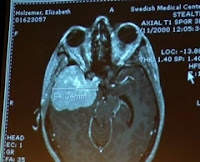
I shouldn't even be writing to you today. Ten years ago, my neurosurgeon informed my husband and me that my baseball sized meningioma should have already put me in a coma and killed me.
As a 10-year meningioma survivor and the founder of the nonprofit, Meningioma Mommas, I can assure you that the thousands of patients we've provided support to would disagree with your inaccurate statement, " this is a meningioma, a benign brain tumor. once removed, patient is cured."
No wonder we have such a struggle getting media attention and funding for this most common primary brain tumor. Dr. Gupta, this is your perfect opportunity to feature meningioma on an upcoming show. I'll be more than happy to put you in touch with thousands of patients, caregivers and family members (and those who have lost a loved one to a so called benign meningioma) who are affected by this disease. I can't think of a better time to educate the world about meningiomas and the more than 120 brain tumors there still is no cure for than during the month of May, which is also the 2nd Annual Brain Tumor Awareness Month.
I also invite you to attend Meningioma Awareness Day in Boston on Oct. 2 where you can meet face to face with hundreds of "cured" patients.
It is a miracle I am alive, but I would hardly consider myself cured especially by the numerous deficits my meningioma has caused. And I am one of the lucky ones.
I look forward to your reply.
Sincerely,
Liz
p.s. If you do read my letter, I urge you to read the following feedback to your tweet from other "cured" meningioma survivors:
"My sister has had 4 meningiomas, I have only had one. Cured after one?"
"If he can't explain himself properly then he should not say anything as it is misleading at the best."
"My daughter has had 2 craniotomys and an additional surgery to implant a VP shunt due to getting Meningitis in the hospital?? We go every 3 months for an MRI. He needs to make a public correction!!!"
"Cured from what?? How unfortunate that he would state something so misleading and insensitive."
"So does that mean my second one wasn't real?? And when they say it will come back that its a lie??? Wow obviously this person has never had or had a loved one deal with this since he can dismiss it so easily!!"
"A prime example of why medical doctors should not use Twitter!!!"
"If I still have 30% of my tumor left and have to endure yearly MRI's would he consider that a cure?"
"How is it possible to be cured if they are unable to remove all of the tumor because it is on your brain stem. Why would we need MRI's yearly if we are cured? Is he saying then that all other doctors that are having us get the MRI's are doing so when there is absolutely no reason to do so (wouldn't that be against their oath?) If the deficits we have, the remaining tumors we have, the regrowths some have are his definition of cured I am afraid that he did not understand anything taught in medical school. The questions we all have when diagnosed and thereafter send us to the Internet in search of understanding. It is a shame that some very unaware and fearful people may end up linking to his FALSE information. I look forward to nothing less than his retraction and apologies for his grossly inaccurate statements."
"What an irresponsible statement for a physician to make. If I was cured 11 yrs. ago after my 1st craniotomy, why did I need Gamma Knife, then 5 yrs later IMRT, then last year a second surgery for three new tumors??? Glad he's not my doctor!!!"
"Why does my left side not work and I have seizures? Makes me angry!"
"Definition of Cure from medterms.medical dictionary
Definition of Cure
Cure: 1. To heal, to make well, to restore to good health. Cures are easy to claim and, all too often, difficult to confirm.
2. A time without recurrence of a disease so that the risk of recurrence is small, as in the 5-year cure rate for malignant melanoma.
3. Particularly in the past, a course of treatment. For example, take a cure at a spa.
The word cure comes from the Latin cura meaning care, concern or attention. The current use of the word cure is believed to reflect the belief that the right care, concern and attention were tantamount to a cure.
Me thinks the good doctor might want to reread his Latin definition for "cura".
"Strange that he thinks seizures, deafness, blindness, etc. etc. are not issues. Must have a 2 month online medical degree."
"Apparently this Dr. never had a family member have this experience..I am 20 months since surgery and deal with sensory and language issues that have completely turned my life in side out. still trying to figure out who I am."
"Really did he ACTUALLY type cured?????"
"I only wish that was true. I am still struggling almost a year after the mass was removed."
"I really wish that was true.. My surgery was almost 2 years ago , I am still having set backs!!!!"
"It is beyond irresponsible for a NS who sees himself as The Great Educator to spread this kind of misinformation when research on this incurable, unpreventable disease is grossly underfunded. To be honest, when I read his tweet I threw up a little bit, in my mouth.
The degree of ignorance about M's amongst NS's is just so frustrating. We see the results of it...day after day with patients being told their symptoms have nothing to do with their brain tumor. What is going on in medical schools? Are they using outdated textbooks? Is it because M's aren't sexy-exciting like lethal GBM's? Is it because they think it's "a women's disease" so they don't care? All of the above?
We have to fight misinformation at every turn, and with ignorance so prevalent it does get tiresome sometimes, but this one, (from the NS who almost became US Surgeon General no less!) is particularly egregious."
"Walk a mile in our meningioma moccasins."